Looking ahead at building personalized experiences for health plans and health systems
2023 Health, Wellbeing, and Benefits Navigation Predictions with Virgin Pulse EVP & GM, Health Plans and Systems, Salem Shunnarah
It’s no secret that healthcare has been facing immense challenges since the COVID-19 pandemic, but things were shifting long before 2020. Consumer healthcare expectations were already at the fore, largely driven by shifts in other industries, such as retail or banking, largely driven by technology. And, while healthcare is a person-to-person industry, we still expect a better experience.
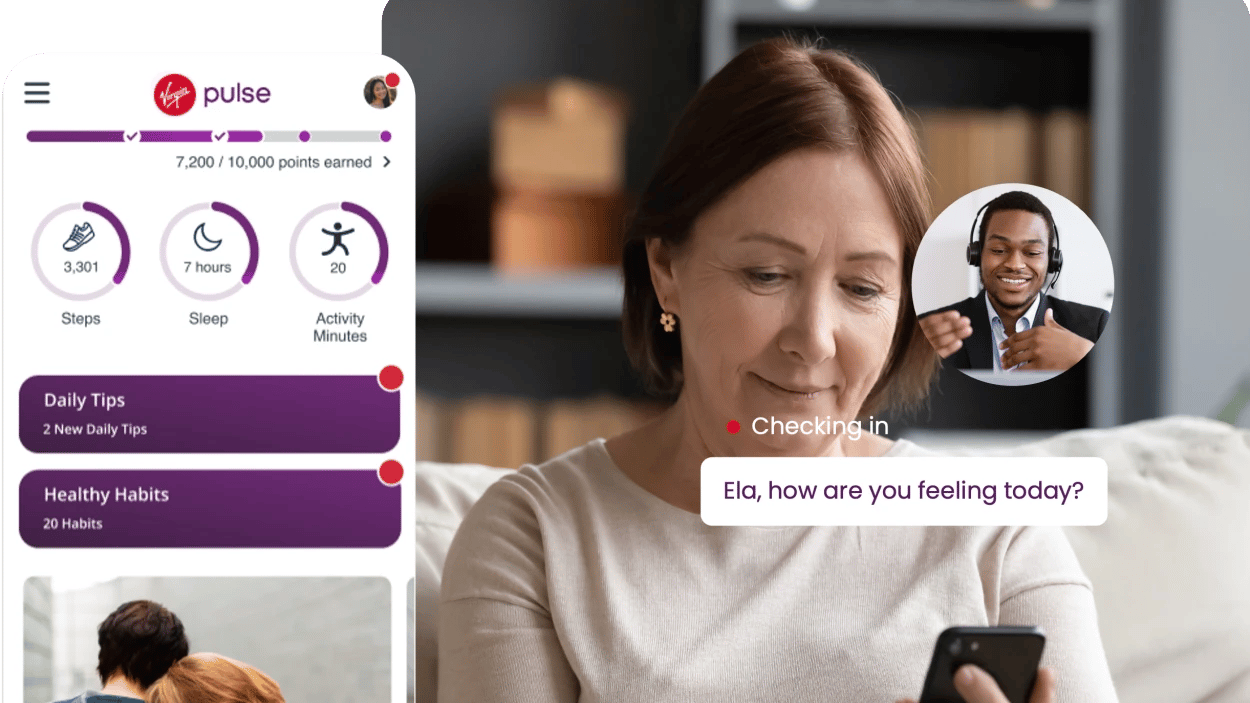
Health plans and health systems are facing pressure to adapt, or they may face declining quality scores and losing patients to other providers. To overcome this challenge, I see health plans and hospitals and health systems embracing a hyper-personalized approach to member/patient engagement over the next few years.
While health plans and health systems don’t have the same goals, similarities and overlaps exist. Both want to drive better health outcomes and improve loyalty–both of which can be accomplished through greater personalization and a better overall experience. Health plans and systems need to recognize that they may think they know their members/patients, but there’s still guesswork involved, and sometimes they get it wrong. The intersection of historical and prospective data - including valuable social determinants of health data (SDOH) - will enable health plans and systems to curate a highly personalized experience for their members/patients, demonstrating that these organizations know who they are and what they need.
In the coming years, I expect many healthcare organizations to take steps to ensure their offerings are culturally competent, relevant, and sensitive to member/patient needs. Heath plans and systems must better understand member demographics and SDOH, such as living in a food desert, having no available transportation, etc. Organizations are just beginning to understand the root causes of healthcare disparities and how to level the playing field – now they must turn up the dial. This is where data plays a critical role. When we understand the nuances, we can more precisely communicate with a population, providing them with a significantly better experience and ultimately improving outcomes. It will be a huge win.
I also expect healthcare organizations to take a more personalized approach to their communications strategies, which can greatly affect the member/patient experience. For example, a person diagnosed as pre-diabetic may not necessarily need intervention – they may already have made some lifestyle modifications (under a doctor’s care) that are working fine. But the health plan continues to contact them with information about diabetes prevention programs, frustrating the member and eroding trust. In the coming years, I foresee organizations embracing more sophisticated communications approaches while giving members the option to opt out and/or communicate back about their preferences – this will help alleviate frustration and help them take better advantage of offerings. By more precisely targeting and communicating with members/patients how they want to be communicated with, health plans and systems will provide a better experience and experience greater loyalty.
Consumer expectations are high, and health plans and systems must rise to meet the challenges. In the coming years, we will see a groundswell across most health plans and health systems embracing new models and data-driven approaches for engagement and communication, providing a better, more personalized experience for their populations. This will help them reach those all-important goals of driving greater loyalty and achieving improved health outcomes.
The Future of Health, Wellbeing, and Benefits Navigation
We've cracked the code on activation and engagement
Turn your vision into action with these related resources.

Member Engagement Playbook for Health Plans
Four expert tips to help you create a VIP Member Experience

5 Trends in Healthcare to Watch Right Now
To realize continued growth and impact, health plans need to stay on top of what’s changing so they can respond. But with so much change, it can be hard to know where to start

Activation & Engagement Solutions for Health Plans & Systems
In a world of increased isolation and distractions, getting and staying connected is a top priority
About Salem Shunnarah
Salem leads customer growth and retention and helps develop value-based products, software, and services for the health plan and health system markets. By aligning market needs and demand with the company’s solutions, the Health Plans & Systems team assists our customers with their strategic and financial goals to drive meaningful activation and engagement via health and wellbeing programs.
Salem brings over 25 years of experience in healthcare, benefits, and human resources, with leadership roles in Fortune 50 consulting and payer organizations, including Anthem and Aon. His experience affords him a deep understanding of the objectives of health plans, employers, and consultants, enabling him to achieve meaningful results. He is driven by his desire to align with customers’ goals to achieve better outcomes while improving the overall healthcare experience

Recent articles
.png?width=1070&height=658&name=Why-Virgin-Pulse-Health-Plans-Health-Activation_03%20(1).png)
Medicaid Redetermination: 5 Reasons Why Texting is Essential for Reaching Members Before it's Too Late